Mar. 03, Wed, 2021
Topics
>RESEARCH
An international collaboration between industry and academia begins with immuno-T-cell therapy using iPS technology!
In January 2021, Juntendo University launched an international collaborative study with Century Therapeutics Inc. to develop allogeneic immune T cells that can fight against refractory malignant lymphoma. Miki Ando, Associate Professor of the Department
of Hematology, School of Medicine, and the leader of the research group behind this study, talked to us about the significance and background of this collaborative study, and shared her thoughts on the future impact of this work.
In 2000, when I joined the Department of Hematology at Juntendo, the first research project I worked on was nasal NK-cell lymphoma caused by EB virus infection. The disease progresses fast, and patients get worse rapidly. In a short period of time, the lymphoma spreads rapidly to all organs in the body, leading to death. Our team was working for developing an effective drug against the disease and we found that L-asparaginase, an anticancer drug commonly used in leukemia, was quite effective. Subsequently, through clinical research by the Japan Clinical Oncology Research Group, anticancer drugs, including L-asparaginase, have become the world’s standard treatment for this type of lymphoma. The drug has increased the survival rate, which was about 10%, to about 50% in one year, but some patients do not respond to the drug or relapse. We wish to continue to explore further lymphoma therapies in order to develop drugs that are effective for such individuals. This aim motivates us to pursue the study of EB virus-associated lymphomas.

 In 2013, I returned to Japan, and joined Professor Hiromitsu Nakauchi at the Institute of Medical Science, University of Tokyo. His group had just developed a technology to rejuvenate T cells using iPS cells, and it was still unknown how the technology
would work against severe viral infections and cancer, and how it could be applied clinically. I joined the research team to create a tumor model for the EB virus and prove how killer T cells derived from iPS cells work against malignant neoplasms. We
found that iPS cell-derived killer T cells are very healthy, more proliferative, and more effective than original killer T cells. In order to pursue full-scale clinical applications for this technology, I returned to Juntendo University. My colleagues
and I obtained samples from patients suffering from cancer, and used them to research whether the killer T cells of interest could be produced.
In 2013, I returned to Japan, and joined Professor Hiromitsu Nakauchi at the Institute of Medical Science, University of Tokyo. His group had just developed a technology to rejuvenate T cells using iPS cells, and it was still unknown how the technology
would work against severe viral infections and cancer, and how it could be applied clinically. I joined the research team to create a tumor model for the EB virus and prove how killer T cells derived from iPS cells work against malignant neoplasms. We
found that iPS cell-derived killer T cells are very healthy, more proliferative, and more effective than original killer T cells. In order to pursue full-scale clinical applications for this technology, I returned to Juntendo University. My colleagues
and I obtained samples from patients suffering from cancer, and used them to research whether the killer T cells of interest could be produced.
※ All T lymphocytes are immune cells. Killer T cells are lymphocytes that recognize viral and tumor antigens and attack abnormal cells.

I must note that the reason Juntendo’s skills are high is because we have many patients collaborating with us as donors. Our patients willingly provide us with blood samples. I almost feel that in the process of repetitively inducing T cell growth from these patients’ cells and producing iPS cells, our techniques eventually refined.

I still remember the excitement I felt during my first research project, when I found out that an unexpected drug worked on refractory nasal NK-cell lymphoma. The fun of nurturing and realizing ideas. The fun of creation. The fun of craftsmanship. Those, I think, are the joys of research.
More than anything else though, the updates we receive from patients play an enormous role in our work. I truly enjoy researching a topic while entertaining the thought that it “might just become a new form of treatment” in the back of my mind. This, too, is all thanks to Juntendo’s translational research environment, where research goes hand-in-hand with treating patients.

Also, because research functions in a team-based fashion, just like clinical practice, it is very important to connect with people. My research team has also grown considerably, but I continue to value teamwork. As a female physician, I have experienced many different life events and have had my own share of struggles. I am forever thankful for the countless people that have supported me in my work thus far.
The goal of this collaborative research project is to produce genome-edited iPS cell-derived killer T cells within 2 years. I get the feeling that this research is going to be the one that finally give rise to a treatment that can be used to treat patients.

Miki Ando
Nasal NK-Cell Lymphoma Leading to Death in the Short Term
Among refractory malignant lymphomas, Epstein-Barr (EB) virus-related lymphoma, caused by infection with the EB virus, has a particularly poor prognosis and is more common in Asia. The EB virus infects between 80% and 90% of adults in Asia, and in most people, all it does is cause cold-like symptoms. However, once infected, the virus remains inside the body for lifetime, and in some cases, it can cause cancer.In 2000, when I joined the Department of Hematology at Juntendo, the first research project I worked on was nasal NK-cell lymphoma caused by EB virus infection. The disease progresses fast, and patients get worse rapidly. In a short period of time, the lymphoma spreads rapidly to all organs in the body, leading to death. Our team was working for developing an effective drug against the disease and we found that L-asparaginase, an anticancer drug commonly used in leukemia, was quite effective. Subsequently, through clinical research by the Japan Clinical Oncology Research Group, anticancer drugs, including L-asparaginase, have become the world’s standard treatment for this type of lymphoma. The drug has increased the survival rate, which was about 10%, to about 50% in one year, but some patients do not respond to the drug or relapse. We wish to continue to explore further lymphoma therapies in order to develop drugs that are effective for such individuals. This aim motivates us to pursue the study of EB virus-associated lymphomas.
Proving the effectiveness of iPS cell-derived killer T cells in the United States and at the Institute of Medical Science, the University of Tokyo
In 2011, I studied abroad at the Baylor College of Medicine, USA, with Dr. Malcom K. Brenner, a well-known authority in the field of gene cell therapy. We were working on a cell death induction system using the suicide gene iCaspase9 (iC9), which targets lung cancer. The team was also conducting research on a variety of other cutting-edge immune T cell therapies. Immune T-cell therapy, which amplifies killer T cells* from the patient’s peripheral blood outside the body and returns them to the patient’s body to attack the tumor, was said to be effective against severe viral infections and cancer. In fact, clinical trials are currently underway for this approach, and I had the privilege of experiencing the effectiveness of this approach firsthand.
Baylor College of Medicine, USA (with Dr. Malcolm K. Brenner and my colleagues from the laboratory)
※ All T lymphocytes are immune cells. Killer T cells are lymphocytes that recognize viral and tumor antigens and attack abnormal cells.
Harnessing healthy donor cells to produce large quantities of healthy and safe killer T cells
T cells produced from cells derived from a patient have the advantage of being less likely to be rejected as they are descended from the patient’s own cells. On the other hand, several patients with cancer have already been treated with anticancer drugs
or radiation therapy; this can cause their cells to grow poorly or to be quite ineffective. In addition, it takes about 5 months to extract cells from the patient and use them to make T cells, and one of our biggest issues was the possibility of the patient’s
condition worsening during that time.
One solution is to produce T cells from cells obtained from another donor; such cells are called allogeneic immune T cells. Blood samples are taken from healthy donors, and the killer T cells produced from them are made into iPS cells. However, they are
foreign invaders for the immune system of a different patient although they are introduced for the treatment of the patient. In order for these killer T cells
to be administered to several patients, even in the presence of immunosuppression, genome editing must be used to modify the cells. It is our goal to produce cells that are safe and reliably effective against tumors and that can be used to treat several
patients.
The technical difficulty of iPS cellularization of killer T cells: Juntendo’s technical skills were recognized and international collaboration started
In recent years, Century, our partner in this collaborative project, has taken on several professional scientists who have been involved in the clinical development of T cell therapies. Thus, as a company, they are able to explore this issue as researchers,
and their aim align with ours: they also wish to develop better T cell therapies. We often use the term “off-the-shelf cell therapy” in conversations with the company; when translated directly into Japanese language, this term basically means that this
product should never go out of stock. It refers to a situation where enough therapeutic cells are available at anytime and anywhere. Producing individualized killer T cells from each patient is time-consuming and costly, as I mentioned previously. However,
if a genome-edited version created from a single iPS cell can be stored ahead of time, and if killer T cells can be produced, we can administer this therapy far and wide and save patients the trouble of waiting for a cure.
Since its inception, Century has also set its sights on off-the-shelf cell therapy. In addition, the company has rated our cells highly, stating “Juntendo’s cells
are of a high technical quality.” The development of allogeneic immune T cells requires various steps, but it is particularly technically difficult to clone the first killer T cell and process it into an iPS cell. Our group is very good at this, and I
think that that is one of the reasons that this collaboration began.
I must note that the reason Juntendo’s skills are high is because we have many patients collaborating with us as donors. Our patients willingly provide us with blood samples. I almost feel that in the process of repetitively inducing T cell growth from these patients’ cells and producing iPS cells, our techniques eventually refined.
Tips from patients become ideas for research
I did not begin my career as a basic research clinician. Originally, I was a hematologist, and I would frequently interact with patients in a clinical setting. As I saw many patients suffering from a variety of diseases, I often pondered why certain diseases
had no cures, or if there might just be other, more effective therapies out there. It was often the case that these questions pushed us to search for answers, which then became ideas for new areas of research. Apart from what we have already achieved,
I think it is important to have a strong desire to “try something new.”
I still remember the excitement I felt during my first research project, when I found out that an unexpected drug worked on refractory nasal NK-cell lymphoma. The fun of nurturing and realizing ideas. The fun of creation. The fun of craftsmanship. Those, I think, are the joys of research.
More than anything else though, the updates we receive from patients play an enormous role in our work. I truly enjoy researching a topic while entertaining the thought that it “might just become a new form of treatment” in the back of my mind. This, too, is all thanks to Juntendo’s translational research environment, where research goes hand-in-hand with treating patients.
The joy of taking on challenges. Your experiences will definitely come in handy!
We recommend that people who aim to be research professionals and clinicians experience a variety of challenges and enjoy every possible aspect of life when they are young. I returned to my research after some time off for childbirth and childcare, and I can say that my past experiences of taking care of patients and spending late nights in the lab, running experiments and writing research papers, have been of great use to me. At that time, I definitely was not thinking that this will come in handy someday. But now, I can say that thanks to my experiences when I was younger, I can roll with the punches easier, in a sense; those long nights in the lab came back as blessings in a way that I had never expected.Also, because research functions in a team-based fashion, just like clinical practice, it is very important to connect with people. My research team has also grown considerably, but I continue to value teamwork. As a female physician, I have experienced many different life events and have had my own share of struggles. I am forever thankful for the countless people that have supported me in my work thus far.
The goal of this collaborative research project is to produce genome-edited iPS cell-derived killer T cells within 2 years. I get the feeling that this research is going to be the one that finally give rise to a treatment that can be used to treat patients.
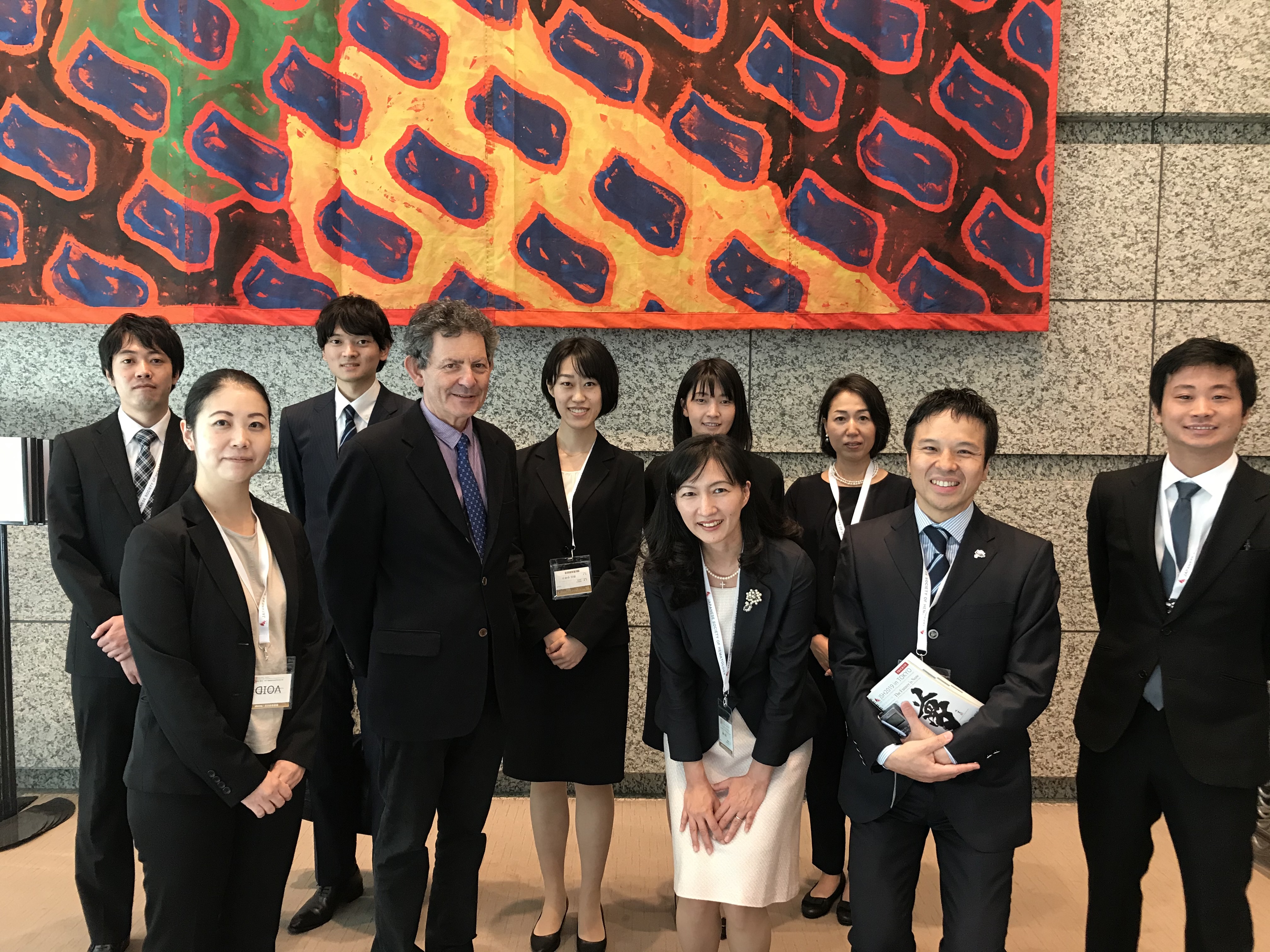
In 2019, Dr. Malcolm K. Brenner was invited to Japan by the Japanese Society of Hematology (Dr. Brenner and laboratory members).

Miki Ando
Associate Professor, Department of Internal Medicine and Hematology, Juntendo University School of Medicine
After joining the Department of Hematology at Juntendo University, Dr. Ando began basic research aimed at developing novel therapies for advanced-stage NK-cell lymphoma. She obtained a PhD in medicine in 2005. In 2011, she became a postdoctoral research
fellow under Professor Malcolm K. Brenner at Baylor College of Medicine in the United States and worked on the development of therapies that apply the apoptosis-inducing suicide gene iC9 to cancer. After returning home, she established a safe iC9 system
for iPS cell-derived CTL therapy under Professor Hiromitsu Nakauchi at the Institute of Medical Science, University of Tokyo. In April 2015, she became a research fellow (RPD) of the Japanese Society for the Promotion of Science, and in April 2016, Associate
Professor of Blood Transfusion and Stem Cell Control at Juntendo University. There, she began preclinical testing of iPS cell-derived rejuvenating CTL therapy for EB virus-associated lymphoma. Since April 2017, she has jointly served as a part-time Lecturer
in the Department of Stem Cell Therapy at the University of Tokyo’s Institute of Medical Science. Since December 2017, she has been working as an Associate Professor in the Department of Hematology at the Juntendo University School of Medicine. In October
2018, her project, “Developing Universal CTL Therapy Derived from iPS Cells for Cervical Cancer” was adopted as an AMED Regenerative Medicine Network Program Technological Development Project. It aims to use genome editing to develop a groundbreaking
treatment modality that can be rapidly implemented in the treatment of large numbers of patients with cancer.